Neck Injuries After an Accident: Symptoms, Diagnosis, Treatment, and Legal Options
Neck injuries after accidents are among the most common—and most underestimated—injuries. These range from whiplash and cervical strains to herniated discs, pinched nerves, and fractures. Symptoms may appear immediately or worsen over 24–72 hours and can include pain, stiffness, headaches, dizziness, numbness, tingling, or arm weakness. Diagnosis may involve a physical exam and imaging such as X-ray, CT, or MRI. Treatment often includes physical therapy and medication, with injections or surgery in severe cases. Compensation may cover medical bills, lost income, and pain and suffering.
Some neck injuries resolve with conservative care. Others cause long-term pain, nerve symptoms, headaches, or disability that disrupts work and daily life. This page explains the major types of neck injuries, warning signs, medical evaluation, treatment options, recovery timelines, and what a personal injury claim may cover.
Quick Answer: What is a “neck injury” after an accident?
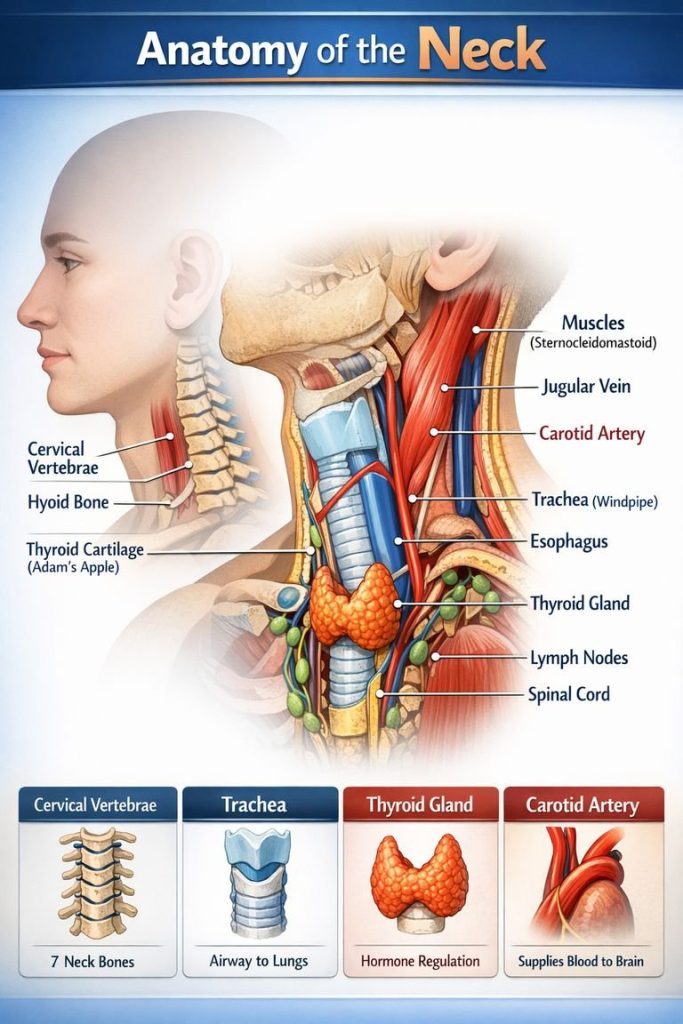
A neck injury is damage to muscles, ligaments, discs, joints, nerves, or bones in the cervical spine (C1–C7) caused by traumatic force—often sudden acceleration/deceleration (“whiplash”), direct impact, or a fall. Neck injuries range from strains/sprains to herniated discs, fractures, and spinal cord injury.
Common causes of neck injuries
Neck injuries can occur in many settings, but these accidents show up most often in injury claims:
- Rear-end collisions (classic whiplash mechanism)
- High-speed car or truck crashes (disc injury, fractures, nerve damage)
- Side-impact (T-bone) collisions (lateral bending/rotation trauma)
- Rollover crashes
- Pedestrian or bicycle impacts
- Slip and falls (head/neck snap, direct impact)
- Workplace incidents (falls, struck-by events)
Types of neck injuries
1) Whiplash (cervical strain/sprain)
Whiplash is a soft-tissue injury to the muscles and ligaments of the neck caused by rapid back-and-forth motion. Symptoms may be mild at first and worsen over 24–72 hours.
Common symptoms
- Neck pain and stiffness
- Reduced range of motion
- Headaches (often starting at the base of the skull)
- Shoulder/upper back pain
- Dizziness, fatigue, “brain fog”
2) Herniated or bulging cervical disc
A traumatic force can injure a spinal disc, causing it to bulge or herniate and irritate nearby nerves.
Common symptoms of whiplash injury
- Radiating pain into the shoulder/arm/hand
- Numbness or tingling (pins-and-needles)
- Weakness in the arm or grip
- Pain that worsens with certain movements or positions
3) Cervical radiculopathy (“pinched nerve”)
When a nerve root is compressed or inflamed—often from a disc injury or bone spurs—pain and neurological symptoms may travel down the arm.
Common symptoms of whiplash injury
- Sharp, burning, or electric pain down the arm
- Tingling/numbness in specific fingers
- Weakness in shoulder/arm/hand muscles
4) Cervical facet joint injury
Facet joints are small joints in the spine that can be damaged by twisting, compression, or whiplash.
Common symptoms of facet joint injury
- Localized neck pain (often one-sided)
- Pain with extension/rotation
- Headaches or pain into the shoulder blade area
5) Cervical fracture or dislocation
More severe crashes and falls can break vertebrae or cause instability.
Common symptoms
- Severe pain, limited movement
- Swelling/bruising
- Neurologic deficits (numbness, weakness)
- Emergency red flags (see below)
6) Spinal cord injury (SCI)
An injury affecting the spinal cord can cause partial or complete loss of function below the injury level. This is a medical emergency.
Neck injury symptoms you should never ignore
Seek urgent evaluation (ER/911) if you have any of these after an accident:
- Weakness in arms or legs
- Numbness in hands, arms, legs, or groin
- Loss of coordination, balance problems, or trouble walking
- Severe headache with neck pain
- Loss of bladder/bowel control
- Confusion, fainting, or repeated vomiting
- Neck pain after a significant impact (especially with midline tenderness)
How doctors diagnose neck injuries
Your medical records matter for both recovery and any injury claim. Common evaluation steps include:
History and physical exam
Clinicians assess:
- Pain pattern and range of motion
- Tenderness, spasm, swelling
- Reflexes, sensation, strength
- Special tests for nerve involvement
Imaging
- X-rays: Can detect fractures, alignment issues, degenerative changes
- CT scans: Better detail for fractures and complex trauma
- MRI: Best for discs, nerves, spinal cord, and soft tissue injuries
Other tests
- EMG/Nerve conduction studies: Sometimes used if ongoing nerve symptoms persist
Treatment options for neck injuries
Treatment depends on the diagnosis, symptom severity, and response over time.
Conservative care (common first line)
- Rest/activity modification (not prolonged bed rest)
- Anti-inflammatory medication (as directed)
- Heat/ice
- Physical therapy (mobility, strengthening, posture, stabilization)
- Home exercise program
Interventional pain management (when symptoms persist)
- Trigger point injections (muscle spasm)
- Epidural steroid injections (disc/nerve irritation)
- Facet injections or medial branch blocks
- Radiofrequency ablation (for certain facet-mediated pain)
Surgery may be considered when there is:
- Progressive neurologic deficit
- Significant spinal cord compression
- Unstable fracture/dislocation
- Severe disc herniation not responding to treatment
Recovery timeline: how long do neck injuries last?
Recovery varies widely. General patterns:
- Mild strains/sprains: days to a few weeks
- Moderate whiplash or disc aggravation: weeks to a few months
- Herniated discs with radiculopathy: months; sometimes longer if nerve irritation persists
- Severe injuries (fracture/SCI): long-term or permanent impairment
Important: Symptoms often flare later, especially after adrenaline fades or swelling increases. Delayed pain is common and does not automatically mean the injury is minor—or unrelated.
Common complications and long-term effects
Some neck injuries lead to lasting problems, including:
- Chronic neck pain and stiffness
- Persistent headaches (cervicogenic headaches)
- Sleep disruption and fatigue
- Reduced ability to work (especially physical jobs or desk work requiring posture)
- Ongoing nerve symptoms (numbness/weakness)
- Anxiety about driving or reinjury (a normal reaction after serious crashes)
What a neck injury claim may include
If your injury was caused by another party’s negligence, a claim may seek compensation for:
- Medical bills (ER, imaging, PT, specialists, injections, surgery)
- Future medical care (ongoing PT, pain management, follow-up imaging)
- Lost income and reduced earning capacity
- Pain and suffering
- Disability or impairment
- Out-of-pocket costs (mileage, braces, home modifications in severe cases)
Evidence that strengthens neck injury cases
Neck injury cases often rise or fall on documentation. Helpful evidence can include:
- Prompt medical evaluation and consistent follow-up
- Objective findings (MRI/CT results, documented neurologic deficits)
- PT records showing functional limitations and progress
- Specialist notes (orthopedics, neurosurgery, pain management)
- Photos of vehicle/property damage and accident scene
- Witness statements and crash report
- Work records showing missed time or job restrictions
What to do after an accident if your neck hurts
- Get checked out—especially with severe pain or neurologic symptoms
- Follow the treatment plan and keep appointments
- Report symptoms accurately (radiating pain, numbness, headaches, sleep issues)
- Avoid “toughing it out” if symptoms are worsening
- Keep a simple pain/function journal (sleep, work limits, daily activities)
- Don’t give a recorded statement to the other insurer without advice
Neck Injuries FAQ
Can whiplash show up days later?
Yes. It’s common for whiplash symptoms to worsen over 24–72 hours after a collision.
Do I need an MRI for neck pain after a crash?
Not always. MRIs are typically ordered when symptoms persist, when there are neurologic complaints (numbness/weakness), or when doctors suspect disc/cord involvement.
How do I know if it’s a pinched nerve?
Radiating arm pain, numbness/tingling, or weakness—especially in a specific distribution—can suggest nerve involvement. A clinician can confirm with exam and imaging.
What if I had arthritis or degenerative discs before the crash?
A prior condition does not prevent a claim. Accidents often aggravate pre-existing conditions. You can recover damages for how much an injury made your condition worse. Medical records and symptom changes are key.
Will the insurance company say it’s “just soft tissue”?
Often, yes—especially early. That’s why consistent medical documentation, functional limitations, and objective findings (when present) matter.
Talk to a lawyer about a serious neck injury
If your neck pain is lingering, radiating into your arm, interfering with work, or worsening over time, it’s worth getting both medical and legal guidance. A personal injury attorney can help gather records, preserve evidence, evaluate future care needs, and negotiate with insurers—so you can focus on recovery.
Call today at (404)253-7862 to schedule a free consultation. We handle car and truck accidents, falls, and serious injury claims, and we only get paid if we win.
Reviewed January 31, 2026 by:
Ken Shigley, senior counsel, former president of State Bar of Georgia, triple board certified by National Board of Trial Advocacy, lead author of eleven editions of Georgia Law of Torts: Trial Preparation and Practice, and received the Traditions of Excellence Award from the State Bar of Georgia General Practice and Trial Section. B.A., Furman University; J.D., Emory University Law School; Certificates in mediation and negotiation, Harvard Law School.
John Adkins, managing partner, experienced in personal injury law, including auto accidents, truck accidents, wrongful death, workers’ compensation, premises liability claims, dangerous or defective products, medical malpractice and related Plaintiff’s tort litigation. B.A., magna cum laude, Kennesaw State University; J.D., Thomas Jefferson Law School.
Ed Stone, partner, personal injury law, including truck accidents, auto accidents, wrongful death, workers’ compensation, premises liability claims, dangerous or defective products, medical malpractice, and related Plaintiff’s tort litigation. B.B.A., Kennesaw State University; J.D., John Marshall Law School.